“We like the fact that with AlignRT, we not only improve setup efficiency but with higher setup accuracy, and with real-time monitoring, we ensure treatment is being delivered safely and accurately.”
Our Market-Leading SGRT Solution
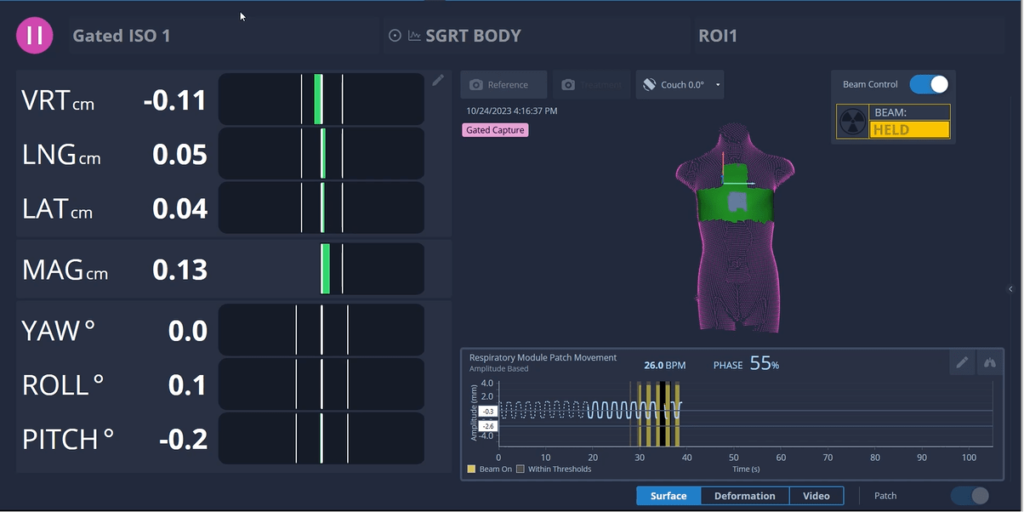
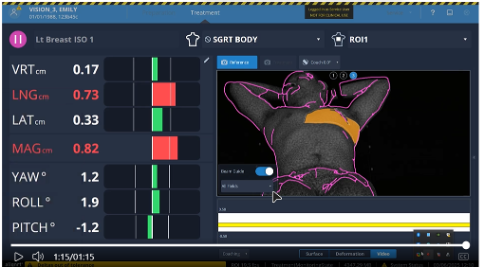
AlignRT is the market-leading Surface Guided Radiation Therapy (SGRT) system, using 3D stereo cameras and 6DoF intrafraction monitoring to ensure radiation is delivered only when the patient is correctly positioned. It provides sub-millimetric accuracy across all skin tones, couch positions, and gantry angles.1-4
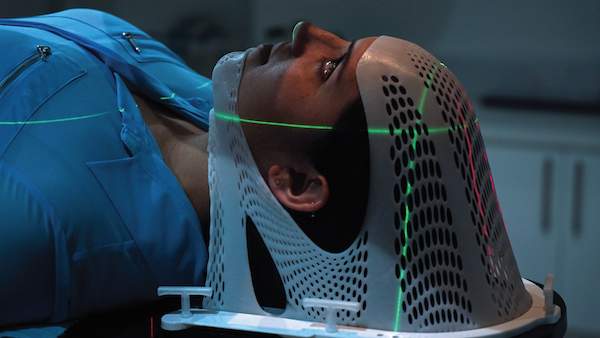
It can automatically pause the radiation beam if the patient moves out of position, and eliminates the need for radiation therapy tattoos or headframes and closed masks for SRS.
AlignRT offers Postural Video™, a patient visualization solution with published evidence showing additional time-savings of 255-1556 seconds per fraction vs standard SGRT.
Built-In Tools
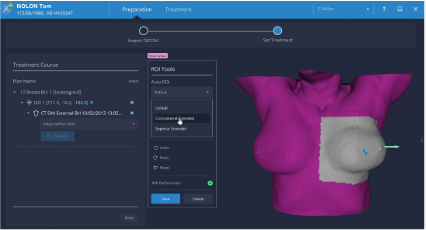
The following tools come standard with the latest version of AlignRT:
A clear, photorealistic image of your patient, to support accurate identification and precise ROI placement.
Provides fast, customizable documentation for treatments, QA, and calibrations enhancing clinical confidence and compliance.
See even the smallest anatomical changes in real time. With intuitive color mapping, the Deformation Tool supports smarter decisions—helping you know when to adjust ROIs or to re-scan.
Get instant insight into ROI performance as you work. AlignRT helps you fine-tune ROI size and shape for optimal tracking and faster setups.
Instantly verify SSDs at a single gantry angle—without the need for manual room checks or other separate processes. Just one click, and you’re ready.
Position patients faster & more accurately with one-click couch value transfers. Eliminates manual entry errors and enables one-step setups. * Available with compatible treatment systems and AlignRT configurations.
Logging into AlignRT is now effortless and secure. Smart Sign-On (using Microsoft’s Active Directory) links to your clinic’s existing credentials to eliminate extra logins, while aligning with your cybersecurity policies. With Smart Sign-On, onboarding new users is fast, automatic, and secure.
Benefits of AlignRT
There are already more than 300 peer-reviewed clinical studies on the effectiveness of SGRT with AlignRT and Vision RT’s systems are being used in 24 of the top 25 “Best Hospitals for Cancer*” in the USA.
| During a study at the University of North Carolina, patients were treated using AlignRT for DIBH. Of these, 0% exhibited radiation-induced abnormalities in blood flow to the heart six months after treatment7. | A study on surface imaging-guided radiosurgery (SIG-RS) found that it offers clinical outcomes comparable to traditional frame-based and frameless SRS techniques for treating brain metastases8. |
| Studies have shown that AlignRT offers sub-millimeter accuracy with real-time measurements and no loss of treatment efficiency9. | AlignRT delivers a tracking accuracy of ≤0.5mm / ≤0.2° at all couch and gantry angles. |
| AlignRT has been shown to reduce treatment times by an average of 22% per fraction.10-16. |
The addition of Postural Video delivers 2517–4018 seconds less setup time per fraction vs. standard SGRT. |
| AlignRT can be used to eliminate the need for tattoos or additional radiation and has been shown to be as accurate as marks or tattoos for positioning patients in preparation for their treatment19-21. | A study published in The Breast Journal22 found that 70% of patients surveyed reported negative feelings about having skin marks during their radiation therapy treatment. |
|
Research suggests that patients often describe closed-face masks as one of the ‘worst’ aspects of their radiation therapy experience23, with nearly half (43%) reporting clinically significant anxiety prior to their mask-making session24. |
Studies have also revealed that patients prefer a tattoo and mark-free option, with 62% of patients feeling negative about tattoos being part of their treatment25. |
Hear from users on their clinical experiences:
-
- Covington EL, et al (2019). Optical surface guidance for submillimeter monitoring of patient position during frameless stereotactic radiotherapy. J Appl Clin Med Phys. 2019 Jun;20(6):91-98.
- Wiant, D et al. (2018). Direct comparison between surface imaging and orthogonal radiographic imaging for SRS localization in phantom. J Appl Clin Med Phys. 2019 Jan;20(1):137-144.
- Sarkar et al. (2018). An evaluation of the consistency of shifts reported by three different systems for non-coplanar treatments. J Radiosurg SBRT.
- Covington, E.L., et al (2020). Surface-guided imaging during stereotactic radiosurgery with automated delivery. Journal of Applied Clinical Medical Physics.
- Oliver, K., Subick, N. and Moser, T. (2025). A prospective, comparative evaluation of an augmented reality tool (Postural VideoTM) vs. standard SGRT for efficient patient setup. Reports of Practical Oncology and Radiotherapy, [online] 29(6), pp.740–745. doi:https://doi.org/10.5603/rpor.104011.
- Holt, D. (2025). Departmental Comparison of AlignRT and Postural Video Versus AlignRT Alone. SGRT Europe 2025 presentation.
- Tanguturi SK, et al., (2015). Prospective assessment of deep inspiration breath-hold using 3-dimensional surface tracking for irradiation of left-sided breast cancer. Pract Radiat Oncol.
- Pan et al. (2012). Frameless, real-time, surface imaging-guided radiosurgery: clinical outcomes for brain metastases. Neurosurgery. 2012 Oct;71(4):844-51.
- Covington, E.L., et al (2020). Surface-guided imaging during stereotactic radiosurgery with automated delivery. Journal of Applied Clinical Medical Physics. J Appl Clin Med Phys. 2020
- Giantsoudi, et al. (2022). Tattoo Free Set-up for Breast Cancer Patients Receiving Regional Nodal Irradiation. Practical Radiation Oncology, Pract Radiat Oncol.
- Mueller, et al. (2023). Accuracy and Efficiency of Patient Setup Using Surface Imaging versus Skin Tattoos for Accelerated Partial Breast Irradiation. Advances in Radiation Oncology.
- Sauer, et al. (2022). Prerequisites for the clinical implementation of a markerless SGRT-only workflow for the treatment of breast cancer patients. Strahlenther Onkol. 2023 Jan;199(1):22-29.
- Wei, et al. (2020). Quantifying the impact of optical surface guidance in the treatment of cancers of the head and neck. J Appl Clin Med Phys. 2020 Jun;21(6):73-82.
- Hickey, et al. (2021). Surface Guided Radiotherapy (SGRT) vs Varian RPM for deep inspiration breath-hold (DIBH) breast treatments. Physica Medica, 84, p.292.
- Kang, et al. (2023). Evaluation of initial patient setup methods for breast cancer between surface-guided radiation therapy and laser alignment based on skin marking in the Halcyon system. Radiation Oncology, 18(1).
- Flores-Martinez, et al. (2020). Assessment of the use of different imaging and delivery techniques for cranial treatments on the Halcyon linac. Journal of Applied Clinical Medical Physics, [online] 21(1), pp.53–61.
- Oliver, K., Subick, N. and Moser, T. (2025). A prospective, comparative evaluation of an augmented reality tool (Postural VideoTM) vs. standard SGRT for efficient patient setup. Reports of Practical Oncology and Radiotherapy, [online] 29(6), pp.740–745.
- Svestad et al., (2025) Setup accuracy and efficiency of real time video assistance for surface-guided positioning in radiotherapy of right-sided locoregional breast cancer. Advances in Radiation Oncology, [online] p.101829.
- Herron et al., (2018). Surface Guided Radiation Therapy as a Replacement for Patient Marks in Treatment of Breast Cancer. International Journal of Radiation Oncology*Biology*Physics, 102(3), pp.e492–e493.
- Shah et al., (2013). Clinical evaluation of interfractional variations for whole breast radiotherapy using 3-dimensional surface imaging. Practical Radiation Oncology, [online] 3(1), pp.16–25.
- Moser et al. (2019). Radiotherapy tattoos: Women’s skin as a carrier of personal memory—What do we cause by tattooing our patients? The Breast Journal, 26(2).
- Kang et al., (2023). Evaluation of initial patient setup methods for breast cancer between surface-guided radiation therapy and laser alignment based on skin marking in the Halcyon system. Radiation Oncology, 18(1).
- Olausson et al. (2017). Development and psychometric testing of an instrument to measure the patient’s experience of external radiotherapy: The Radiotherapy Experience Questionnaire (RTEQ). Technical Innovations & Patient Support in Radiation Oncology, 3-4, pp.7–12.
- Burns, M., Campbell, R., French, S., Dhillon, H.M., Butow, P.N., Pritchard, A. and Sundaresan, P. (2022). Trajectory of anxiety related to radiation therapy mask immobilization and treatment delivery in head and neck cancer and radiation therapists’ ability to detect this anxiety. ‘Anxiety during radiation therapy with mask’. Advances in Radiation Oncology, p.100967.
- Moser, et al. (2019). Radiotherapy tattoos: Women’s skin as a carrier of personal memory—What do we cause by tattooing our patients? The Breast Journal, 26(2).
*Ranked by U.S. News & World Report.
Get in touch
Ready to take the next step?
Vision RT’s family of SGRT solutions guide radiation therapy for better patient care at every step: Sim, Planning, Treatment and Dose. Whether you’re looking for a quote, a product demo (virtual or in-person) or just more information, please get in touch.